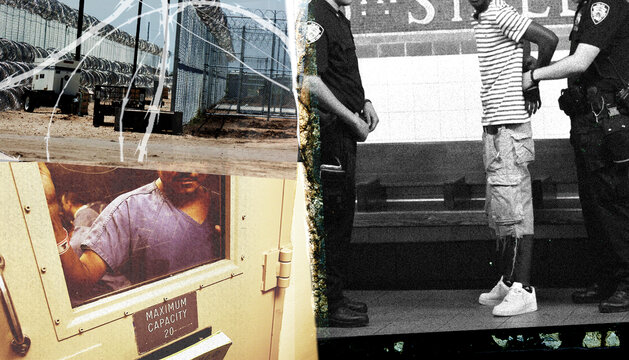
Covid-19 and the Struggle for Health Behind Bars
For many, harming the health of people in prison appears to have become part of their punishment. That needs to change.

Part of
This essay is part of the Brennan Center’s series examining the punitive excess that has come to define America’s criminal legal system.
A little more than a year ago, I left my job as president of a nonprofit so I could respond full time to the spread of Covid-19 in jails, prisons, and immigration detention centers. Since then, I’ve conducted about 30 inspections of facilities to assess their Covid-19 responses and provide recommendations.
How do things look from this perspective? Are we any closer to building systems and cultures that promote health in these settings, instead of harming the health of the incarcerated to such a degree that it actually becomes a part of punishment? When I compare Covid-19 to past health crises in carceral settings, I’m concerned that we will simply improve care delivery for one disease instead of using this moment to push for transparency about all health risks and health outcomes behind bars.
The Centers for Disease Control and state health departments are currently engaged in carceral settings, but their gaze will soon shift once vaccines have been delivered and rates of Covid-19 abate. We must keep their focus there, to learn and report on the truth of health care access, adequacy, and outcomes just as they do for the rest of our society.
Now, some notes from the field. As of June, most of the attention regarding Covid-19 behind bars is focused on vaccination efforts, with good reason. Starting in January, vaccines became widely available to most correctional staff. For detained people, access started in waves in February and March. Low acceptance rates among correctional staff created a surplus of available vaccine in many facilities, enabling even more detained people to become vaccinated. By March and April, the low vaccination rate among correctional staff was a national problem, and many prisons, jails, and detention centers were struggling to exceed a vaccination rate of 40 percent among staff, while achieving vaccination rates over 60 percent among detained people.
But in some institutions, the way vaccines are offered — usually to large groups of individuals, for example everyone in a housing area or dining hall — is itself a problem. This approach often leaves little room for people with questions about vaccine safety or complex medical problems to ask their own questions about vaccination. As a result, some of the people who need the vaccine the most, like those who have multiple serious health problems and those who are taking numerous medications, end up not being vaccinated simply because they are denied the opportunity to learn what they wish to know.
Both of these vaccination challenges — the hesitancy of correctional staff and the deficiencies of the assembly line approach to vaccination of the detained — can be addressed with engagement. An engagement approach, which entails eliciting the individual’s input and participation in his or her health care, is standard for community health clinics, hospitals, and other health organizations. But in jails, prisons, and immigration detention facilities, the very notion of individualized engagement can be seen as a threat to the paramilitary approach of corrections.
For example, a common response to a patient exhibiting suicidal behavior is to lock them in a cell, naked except for a rough “suicide smock,” with the goal of depriving them of the means to harm themselves. This approach not only fails to address the actual mental health crisis but also adds additional humiliation and isolation for a person who desperately needs treatment and engagement.
Some penal systems are working to increase Covid-19 vaccine engagement via one-on-one meetings with high-risk patients. These sessions are often added into the preexisting visits that people with chronic health problems already have, so as to target high-risk patients who may have questions about their health problems, medications, and Covid-19 vaccines. Some law enforcement agencies have also conducted surveys of their staff to understand attitudes and reluctance and to provide incentives for vaccination. But most American correctional health services remain under the authority of security forces, which often have little appetite for public health and infection control.
Much of the current focus in the battle against Covid-19 behind bars has been to identify the morbidity and mortality of the disease among a vulnerable group of people. But this work has also identified the numerous weaknesses in care and conditions before Covid-19, including failing sick call and chronic care systems and lack of consistent access to specialty care and medications.
The most damning failure illuminated by Covid-19 is how the CDC and state departments of health are essentially AWOL when it comes to tracking health outcomes or providing objective assessments of the quality of care for people behind bars. For hospitals, nursing homes, and many other cohorts of our society, these are tasks that both state departments of health and the CDC perform routinely, and with great skill — but not in carceral institutions. The CDC created helpful Covid-19 guidelines early in the pandemic, but it has almost no involvement in tracking actual adoption of those recommendations, nor does it even aggregate statistics about deaths and illness from Covid-19 in carceral settings.
And despite clear evidence of the increased risk of illness and death from Covid-19 behind bars, the CDC has been all but silent on the most effective tool: release. Release of high-risk patients has been essential to protect the most vulnerable people from serious illness and death from Covid-19, and it has also been critical to allowing facility administrators the room to establish medical isolation and quarantine units when the need arises.
This lack of oversight and interest among our national and state health bodies has reinforced the horrible reality that harming health is part of the punishment of incarceration. People are routinely incarcerated with and even because of health problems for which they will never receive treatment; instead, they are exposed to new health risks that can cause them to suffer serious illness, long term disability, or death.
For example, people arrested on substance use-related charges rarely receive evidence-based treatment for that health problem. In many communities, the primary response to a mental health crisis is the same: incarceration in a local county jail. These behavioral health problems lead to incarceration for people of color, those who are poor, and especially those who are uninsured, yet these same health problems are unlikely to be treated appropriately, causing many jail deaths.
I recently told European colleagues working on Covid-19 about two aspects of our system that shocked them — and should shock all of us into action. The first was that the most recent data on deaths in U.S. jails dates from 2016. Just recall the controversy over how deaths from Covid-19 were reported in New York nursing homes; imagine waiting five years to learn of those deaths. The second shocker: Covid-19 is estimated to have reduced the life expectancy of prisoners in Florida’s state system by four years. Both of these facts indict a national public health apparatus that has turned its back on incarcerated people, inevitably widening racial disparities in the process.
We must make an affirmative decision to apply the same lens of health expertise and transparency to carceral settings as we do to other parts of society. Concretely, we can begin to address this failure by setting up an office of detention health in the CDC that is charged with tracking the health of incarcerated people nationwide and the care provided them. In fact, this is one of the many interim recommendations recently made by the Biden-Harris Health Equity Task Force (which I am a member of) to involve the CDC in tracking health outcomes and promoting health among incarcerated people.
With federal support, the same monitoring process could be used in state health departments, and then we can join the effort to measure how incarceration harms health, how carceral settings should provide health care, and how undoing mass incarceration can improve individual, family, and community health.
The CDC has a lot of work to do in this realm, and it can start by looking at the rates of “long Covid,” determining the efficacy of release and other Covid-19 responses during the pandemic, getting involved in suicide prevention (still the number one cause of death among the incarcerated), and analyzing the health needs (and costs of care) of the enormous and growing portion of elderly people behind bars.
These minimal interventions are crucial for improving our response to Covid-19, as well as the next pandemic, and for informing the nation of public health problems that arise from mass incarceration. They are also small but necessary steps towards addressing the reality that harming health is not a byproduct of incarceration but, seemingly, one of its objectives.
Dr. Homer Venters is a member of the Biden-Harris COVID-19 Health Equity Task Force and former chief medical officer of NYC Correctional Health Services. He is an epidemiologist and a clinical associate professor at the New York University College of Global Public Health. Unless otherwise stated, his opinions are presented here as his own.
More from the Punitive Excess series
-
Collateral Consequences and the Enduring Nature of Punishment
For some people, punishment can continue years after the sentence ends, even decades. -
Probation and Parole as Punishment
Community supervision must be transformed in order to help people caught up in the justice system, not hurt them further. -
The Dehumanizing Work of Immigration Law
America’s immigration rules are unduly harsh, leading to family separation and other needless suffering.